A shoulder fracture can be a painful and debilitating experience, impacting daily life and independence. Understanding the immediate shoulder fracture symptoms is the first step toward seeking timely and appropriate medical care. In this post, we’ll take a close look at the signs to look for, along with the diagnostic process and the various treatment pathways available.
Key Takeaways
- The primary shoulder fracture symptoms include sudden, intense pain, swelling, bruising, and an inability to move the arm. A visible deformity or a grinding sensation (crepitus) may also be present.
- Fractures most commonly affect the clavicle (collarbone) and the proximal humerus (the top part of the upper arm bone). Scapular (shoulder blade) fractures are less common and often associated with high-energy trauma.
- Diagnosis relies on a thorough physical examination and imaging studies, typically starting with X-rays.
- Many shoulder fractures are treated non-surgically with immobilization (sling) and physical therapy. However, displaced or unstable fractures may require surgical intervention to restore alignment and function.
The Anatomy of a Shoulder Fracture
The shoulder is a sophisticated arrangement of bones, muscles, tendons, and ligaments. A fracture is a break in any of the three bones that make up the shoulder joint: the clavicle, the scapula, or the proximal humerus. Shoulder fractures may be classified as non-displaced, where the bone remains properly aligned, or displaced, where the broken pieces shift out of position and may require more involved treatment to restore normal alignment.
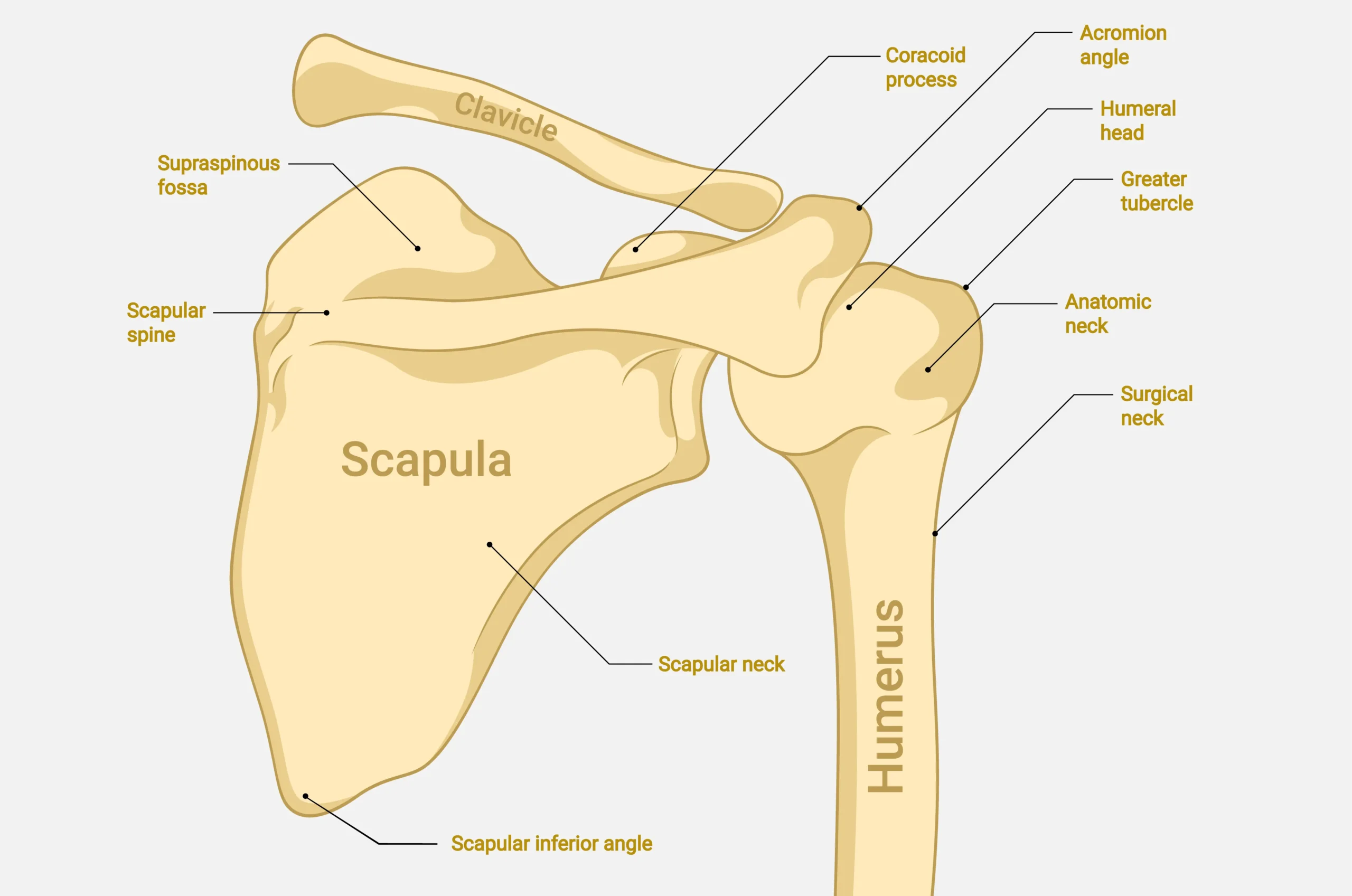
The Proximal Humerus
The proximal humerus is the rounded top section of the upper arm bone. It fits into the socket of the scapula, forming the ball-and-socket joint. Fractures here are common, especially in older adults with osteoporosis, frequently resulting from a simple fall onto an outstretched arm.
The Clavicle (Collarbone)
The clavicle is a long, slender bone that connects the arm to the trunk of the body. It acts as a strut, keeping the shoulder in the correct position. Clavicle fractures often occur after a fall directly onto the shoulder or a blow to the area.
The Scapula (Shoulder Blade)
The scapula is a large, flat, triangular bone located on the back of the rib cage. Because it is well-protected by a thick layer of muscle, a scapular fracture is rare. When it does occur, it is usually the result of a high-energy trauma, such as a motor vehicle accident or a significant fall.
Recognizing Shoulder Fracture Symptoms
The presentation of a fractured shoulder can vary depending on the bone involved and the severity of the break. However, certain shoulder fracture symptoms are present in most cases.
Primary Indicators of Injury
The most immediate sign of a fracture may be sudden, severe pain. This pain is typically localized to the shoulder area and is dramatically worsened by any attempt to move the arm. The intensity of the pain often prevents the patient from moving the arm at all.
Swelling and bruising are also common shoulder fracture symptoms. The area around the fracture site may quickly become swollen as blood and fluid accumulate. Bruising may appear rapidly and can extend down the arm or across the chest wall. The extent of the bruising does not always correlate with the severity of the fracture.
A grinding or popping sensation, medically termed crepitus, may be felt or heard when the patient attempts to move the injured arm. This sensation is caused by the fractured bone ends rubbing against each other.
Functional and Visual Symptoms
The inability to use the arm is a significant functional symptom. Patients often hold the injured arm close to the body, supporting it with the uninjured hand. This is a natural splinting mechanism.
In cases of displaced fractures, a visible deformity may be apparent. The shoulder may look “out of place,” or a bump may be visible where the bone has broken and shifted. For a clavicle fracture, the shoulder may sag downward and forward.
It is important to remember that many of these symptoms are not exclusive to fractures. A severe sprain, dislocation, or rotator cuff tear can present with similar signs. Therefore, a diagnosis often requires professional medical evaluation.
The Diagnostic Process
When a patient presents with classic shoulder fracture symptoms, the diagnostic goal is to accurately identify the location, type, and severity of the fracture, which is important for determining the correct treatment.
Your doctor will first take a detailed history of the injury, asking about how the injury occurred. This information can provide clues about the potential fracture pattern. The physical examination is then conducted with great care to avoid causing further pain or injury.
X-rays are typically the standard initial imaging study. They provide clear images of the bone structure. Multiple views may be taken to visualize the fracture from different angles, which helps the surgeon understand the degree of displacement and angulation.
For more complex injuries, or when the fracture involves the joint surface (glenoid), a CT scan may be ordered. A CT scan provides detailed, cross-sectional images of the bone, which can be valuable for surgical planning. In some cases, especially when soft tissue injury is suspected alongside the fracture, magnetic resonance imaging (MRI) may be used.
Treatment Options for Shoulder Fractures
The treatment for a shoulder fracture is highly individualized. It depends on the patient’s age, activity level, overall health, and, most importantly, the type and displacement of the fracture. The two main categories of treatment are non-surgical (conservative) and surgical.
Non-Surgical Treatment
The first step is often to immobilize the shoulder to allow the bone fragments to heal. This is typically achieved with a sling or a specialized shoulder immobilizer. The duration of immobilization ranges, depending on the fracture type and the patient’s healing rate.
Pain control is important, especially in the initial days following the injury. This may involve a combination of non-steroidal anti-inflammatory drugs (NSAIDs) and, in some cases, short-term use of stronger pain medication. Ice application is also a simple way to help reduce pain and swelling.
While immobilization is frequently necessary, prolonged rest can lead to shoulder stiffness. Therefore, a carefully timed and structured physical therapy program typically begins with gentle, passive range-of-motion exercises, often starting within the first few weeks. The goal is to prevent stiffness and gradually restore strength and full function.
Surgical Treatment
Surgery is generally reserved for fractures that are significantly displaced, unstable, or involve the joint surface in a way that would lead to poor function or early arthritis if left untreated.
Open Reduction and Internal Fixation (ORIF): This procedure involves the surgeon making an incision to access the fracture site. The bone fragments are then carefully realigned and held in place with metal hardware, such as plates, screws, or pins (internal fixation).
Arthroplasty (Joint Replacement): In cases of severe proximal humerus fractures, or when the blood supply to the humeral head is compromised (avascular necrosis risk), the recommended option may be to replace the joint. Reverse shoulder replacement is often used for complex fractures in older patients, especially those with pre-existing rotator cuff deficiency. The ball and socket are reversed, which allows the deltoid muscle to power the arm, bypassing the need for a functional rotator cuff.
The decision to proceed with surgery is a complex one, involving a careful discussion between the patient and an expert orthopedic surgeon about the risks, benefits, and expected outcomes of each option.
The Recovery and Rehabilitation Journey
Full recovery can take six months to a year or longer, depending on the fracture and treatment plan. The timeline varies widely, but a general recovery framework can be outlined, broken into phases.
Phase 1: Immobilization and Early Motion
This initial phase focuses on pain control and protecting the fracture site. The arm generally remains in a sling or immobilizer. For non-surgical cases, or after the initial post-operative period, the surgeon may recommend very gentle, passive range-of-motion exercises. These exercises are performed by the therapist or the patient’s uninjured arm, ensuring the shoulder muscles remain relaxed. The goal is to prevent the formation of scar tissue and maintain mobility.
Phase 2: Active Range of Motion
Once the surgeon confirms initial bone healing, the patient may begin active range-of-motion exercises. This means the patient starts moving the arm using their own muscles. The exercises become more challenging, focusing on restoring the full arc of motion. The patient may work on lifting the arm forward (flexion) and out to the side (abduction).
Phase 3: Strengthening
This phase is dedicated to rebuilding the strength and endurance of the shoulder muscles, particularly the rotator cuff and the deltoid. Resistance exercises, often starting with light bands and progressing to weights, may be introduced. The focus often includes functional movements, preparing the patient to return to daily activities, work, and sports.
Summary
Recognizing the key shoulder fracture symptoms, intense pain, swelling, and loss of function, is the first step toward management. Whether the treatment involves a simple sling or surgery, the ultimate goal is the restoration of a pain-free and functional shoulder. By understanding the anatomy, the nature of the injury, and the commitment required for rehabilitation, patients can partner effectively with their orthopedic team to navigate the recovery process.
Frequently Asked Questions
Can a shoulder fracture heal without surgery?
Yes, some shoulder fractures, particularly those that are non-displaced or minimally displaced, can heal successfully without surgery. Non-surgical treatment frequently involves immobilizing the arm in a sling and then beginning a structured physical therapy program once the initial healing has occurred. Surgery is typically reserved for fractures that are displaced or unstable.
What is the difference between a shoulder fracture and a shoulder dislocation?
A shoulder fracture is a break in one of the bones of the shoulder (humerus, clavicle, or scapula). A shoulder dislocation occurs when the head of the humerus (the ball) is forced out of the glenoid (the socket). While they are distinct injuries, they can sometimes occur together.
What should I do immediately after I suspect a shoulder fracture?
If you suspect a shoulder fracture, it can help to immobilize the arm as best as possible. Consider applying ice to the area for 15-20 minutes at a time to help reduce swelling and pain. Seek medical attention at an emergency room or an orthopedic urgent care center. Do not attempt to move the arm or “pop” the shoulder back into place, as this could cause further damage.
How can I sleep comfortably with a fractured shoulder?
Sleeping with a fractured shoulder can be challenging. Many patients find it most comfortable to sleep in a semi-reclined position, such as in a recliner chair or propped up in bed with several pillows. This position often reduces the pull of gravity on the fracture site. You should continue to wear your sling or immobilizer as instructed by your doctor, even while sleeping, to prevent accidental movement. Placing a small pillow behind the elbow for support can also help.