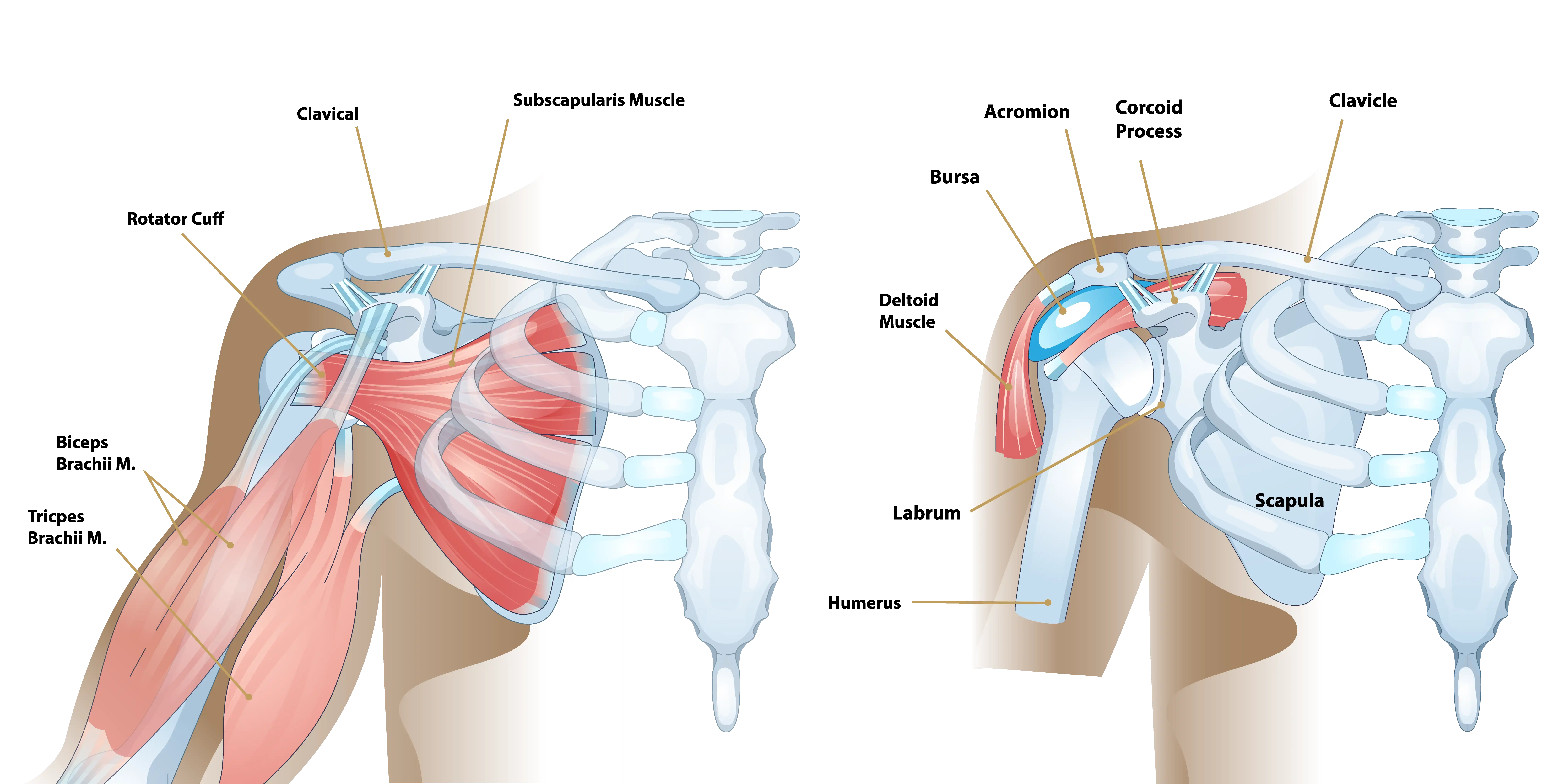
Your shoulder is the most flexible joint in your body, allowing you to throw fastballs, lift a heavy suitcase, scratch your back, and reach in almost any direction. However, its extreme mobility comes at a cost, as the shoulder is prone to instability. Your shoulder joint is like a ball in a small shallow saucer. The ball, or head, of the arm bone (humerus) rests in the shoulder socket (glenoid). The soft tissues of the shoulder act like stabilizers to hold the humeral head and glenoid together and keep the joint stable.
Anatomy of the Shoulder
The humeral head is the rounded top part of your upper arm bone, and it fits into the glenoid, which is the socket of your shoulder blade. Surrounding this joint is the rotator cuff, a group of muscles and tendons that stabilize the shoulder and allow it to move. Muscles are soft tissues that span the joint and help move bones, while tendons are strong, cord-like fibers that attach muscles to bones.
The joint capsule is a tough, fibrous envelope that encloses the humeral head and glenoid, forming a sealed “bag” that holds in joint fluid for lubrication. Lining the edge of the glenoid is the labrum, a ring of tough, flexible cartilage that deepens the socket and helps attach the capsule to the glenoid, providing additional stability.
Because your shoulder joint is so flexible, your arm may move too far, pushing the humeral head completely out of the glenoid. This is called a dislocation. When the head is pushed only partway out of the glenoid and returns to normal on its own, it is called a subluxation. Subluxing or dislocating your shoulder can stretch or tear your capsule and damage other parts of the joint. This makes the humeral head more likely to slip out of the glenoid again. Here are types of damage that can cause instability.
Dislocations & Subluxations of the Shoulder
Dislocations can Tear the Capsule
When the humeral head pushes out of the glenoid, the capsule can tear. The torn capsule cannot stop the humeral head from moving out of the glenoid, so the humeral head may slip out repeatedly.
Dislocations can Damage the Glenoid and Humeral Head
When your shoulder dislocates, the humeral head can hit the glenoid rim, fracturing the glenoid and denting the humeral head. This damage makes the humeral head more likely to slip out of the glenoid again and again. Over time, this bone and cartilage loss can accelerate, leading to early arthritis.
Subluxations can Stretch the Capsule
If your humeral head pushes only partway out of the glenoid, the capsule may stretch rather than tear. The stretched capsule is too loose to stop the humeral head from leaving the glenoid when you raise your arm.
Dislocations and Subluxations can Tear the Labrum
When the humerus pushes all or partway out of the glenoid, the humeral head can tear the labrum. Since the labrum helps hold the humeral head the glenoid, a torn labrum mean the humeral head may slip out of the glenoid.
Shoulder instability develops in two different ways: traumatic (injury related) or atraumatic. Understanding the differences is essential in choosing the best course of treatment. Traumatic instability begins when an injury causes a shoulder dislocation. The patient with atraumatic instability has general laxity (looseness) in the shoulder joint that eventually causes the shoulder to become unstable.
Traumatic shoulder instability is most common in young, athletic people. The younger and more active the patient is when the first dislocation occurs, the more likely it is that recurrent instability will develop. For example, if the first dislocation occurs during the teenage years, there is a 70% chance that recurrent instability will develop. However, people over age 50 with a first dislocation have less than 10% risk of developing chronic instability. Treatment strategies should be designed to suit each patient’s age and lifestyle.
What is traumatic shoulder instability?
Traumatic shoulder instability begins with a first dislocation that injures the supporting structures of the shoulder. The glenoid (the socket of the shoulder) is a relatively flat surface that is deepened slightly by the labrum, a cartilage cup that surrounds the glenoid and contacts part of the head of the humerus. The labrum acts as a bumper to keep the humeral head firmly in place in the glenoid. More importantly, the labrum is the attachment point for ligaments stabilizing the shoulder. When the labrum is torn from the glenoid, the support of these ligaments is lost.
The development of recurrent instability depends upon the type and amount of damage that is done to the labrum and the supporting ligaments. The most common dislocation that leads to traumatic instability is in the anterior (forward) and inferior (downward) directions.
A fall on an outstretched arm that is forced overhead, a direct blow of the shoulder, or a forced external rotation of the arm are frequent causes of this type of dislocation. Much less common is a posterior (backward) dislocation, which is usually related to a seizure disorder or electrocution, events in which the muscular forces of the shoulder cause the dislocation.
What are the signs and symptoms of a dislocation?
If the shoulder is dislocated, it is usually very apparent:
- The shoulder is quite painful
- Motion is severely restricted
- The shoulder appears to hang down and forward, with a large dimple evident under the acromion (in the collar bone area).
The humeral head may be visible as a bump on the front of the shoulder, or in the armpit. To return the dislocated arm to its socket (called a reduction) usually requires a visit to the emergency department, where expert assistance can be found. Some individuals with recurrent dislocations eventually become experienced at reducing the arm themselves.
How is dislocation and traumatic shoulder instability diagnosed?
As a rule, a sudden dislocation is quite evident. The patient usually holds the arm against the side, since any attempts at motion cause pain. A large crease under the acromion and a bulge in the armpit are clues to the direction of the dislocation. However, when the shoulder spontaneously relocates into its proper position, the diagnosis can be more difficult. Patients may only report the feeling of having the shoulder “slip” or “shift” before the spontaneous reduction occurred.
A qualified individual usually can relocate the humerus at the site of the injury occurrence. Once the reduction is performed, there is immediate pain relief. Without medications, some patients may be unable to relax the shoulder muscles enough to allow the reduction to take place. Often these patients must go to the emergency department to get the reduction accomplished.
X-rays are usually taken to confirm the dislocation, its direction, and to check for a related fracture. After the reduction, follow up X-rays will confirm proper positioning and assess any other injuries to the bones. X-rays may reveal a “bony Bankart”, which is a fracture of the anterior-inferior glenoid (front, lower portion of the glenoid). The presence of this fracture indicates that the labrum and ligaments in the front part of the shoulder are no longer attached to the glenoid.
Frequently, an MRI-arthrogram may be ordered (MRI with a contrast dye injected into the joint to improve accuracy). In this diagnostic test, the status of the labrum and ligaments can be assessed. A Bankart lesion (detachment of the anterior-inferior portion of the labrum from the glenoid) is the most common cause of recurrent instability after an injury.
How is a dislocation and traumatic shoulder instability treated?
The initial reduction of a dislocation can be quite difficult. Contractions of the shoulder muscles can trap the humeral head outside of the glenoid. Gentle traction, and at times, medication or sedation may be needed to accomplish the reduction. Once the shoulder is reduced, a sling is used to protect the shoulder and relieve discomfort. A period of immobilization with sling use is generally recommended for 4 weeks following the dislocation followed by physical therapy.
Non-Operative Treatment
Initial treatment for recurrent instability for the shoulder usually includes physical therapy unless there exists a high risk of failure of non-surgical treatment. Strengthening the rotator cuff muscles and periscapular muscles (those around the scapula) helps to improve stability in the joint. The goal of physical therapy is to help the muscles provide stability to the shoulder that the torn ligaments or labrum can no longer supply.
The therapy for recurrent instability shoulder be carefully designed for each patient since this condition often causes apprehension about certain arm position or exercise maneuvers. Very often, physical therapy can help regain lost motion, reduce apprehension, and restore shoulder function.
Operative Treatment
Surgery is usually recommended if recurrent instability cannot be controlled with physical therapy and activity modification or in some patients who carry a high risk of recurrent dislocations. Patient age, activity demands, the presence of bone loss, and certain structural defects can lead to failure of nonsurgical treatment. The goal of surgery is to return stability to the shoulder with the least loss of motion.
All shoulder procedures designed to stabilize the shoulder can cause some loss of motion. The current procedures for anterior shoulder instability attempt to restore the normal anatomy without over tightening the ligaments. In certain instances, such as in young patients who have a higher risk of re-dislocation and in contact athletes who plan on continuing to participate in sports that put their shoulder at risk, surgery may be performed after the first dislocation.
Surgical Procedures for Shoulder Instability
Open Labral Repair
Historically, the preferred procedure for treating anterior instability was an open labral repair with an anterior capsular shift. This procedure is performed through a two to three-inch incision on the front of the shoulder. The torn labrum is repaired and the stretched-out anterior shoulder capsule is imbricated (overlapped) to make it smaller.
This procedure was very successful in eliminating recurrent dislocations, however has now been replaced by minimally invasive arthroscopic techniques which also provide excellent outcomes. Some cases with significant bone loss are treated more successfully with an open procedure developed in France called the open Latarjet procedure.
In this procedure, bone from the coracoid process and the attached conjoined tendon are transferred to the glenoid in order to address the bone loss and instability problem.
Arthroscopic Techniques
Recently, arthroscopic procedures such as an arthroscopic Bankart repair have been used to repair the torn labrum and reduce capsular laxity. Arthroscopic techniques are approximately 90% successful. These procedures are performed with visualization through a small fiberoptic scope.
Instruments are inserted into the joint through two or three small incisions to repair the labrum. The surgical technique is like the one used in an open repair. Procedures using thermal energy to shrink the loose capsule are no longer recommended.
Potential Complications
The major complications of anterior stabilization techniques are recurrent instability and/or some loss of motion. The rate of recurrent instability depends largely on the technique used for the repair. In general, the operative shoulder should lose no more than ten degrees of external rotation. Other small risks (less than 1%) include infections, post-operative stiffness, nerve damage, or blood vessel injury.
Recovering from Shoulder Instability
Non-Operative Recovery
Patients who have a first dislocation, and do not develop recurrent instability, will often regain full motion from a four to six-week course of physical therapy. Patients who do develop recurrent instability have a longer rehabilitation course and should concentrate on strengthening the shoulder muscles. Daily exercises in a home program may be recommended to help prevent instability events.
Operative Recovery
Following either arthroscopic or open operative repair and stabilization, the patient will usually wear a sling for the first four to six weeks. The immobilization protects the repaired labrum while it heals to the glenoid. Until the ligaments heal, the repair must depend on the sutures used to secure the labrum. During this immobilization period, elbow and wrist motion are maintained with gentle range of motion exercises.
Physical therapy begins within 2 weeks of surgery. This is very important. Exercises stressing range of motion are done for approximately 8-10 weeks after surgery, and strengthening begins at 3 months following surgery. Overhead sports, such as baseball or tennis, may resume after about five months after surgery. Contact sports are restricted for six months.
Summary
The shoulder’s remarkable range of motion allows for a wide variety of movements but also makes it vulnerable to instability, especially following traumatic injury. When the shoulder dislocates or subluxes, key stabilizing structures—such as the capsule, labrum, and bone—can be damaged, increasing the risk of future dislocations.
Early and accurate diagnosis, along with a treatment plan tailored to the patient’s age, activity level, and degree of joint damage, is critical for restoring function and preventing recurrence. Whether managed through physical therapy or surgical intervention, the ultimate goal is to return the shoulder to a stable, pain-free state while preserving as much motion and strength as possible.
If you’re experiencing shoulder instability or have suffered a dislocation, it’s important to discuss your treatment options with an expert. Dr. John Costouros, a specialist in shoulder surgery, can help you understand your condition and develop a personalized plan to restore strength, stability, and confidence in your shoulder.